The Current Progress of Nipah Virus Vaccine Development
Nipah Virus (NiV) and its Effects on Humans
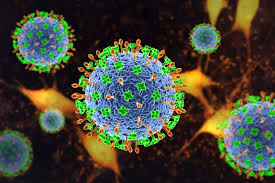
Nipah Virus (NiV) is a potentially fatal zoonotic virus with the potential to cause disease outbreaks in both humans and animals. It was first discovered in 1998 in Malaysia, when pigs were found to be infected with the virus after the outbreak of a respiratory illness in humans near a pig farm. NiV is highly contagious and can be spread from person-to-person, through contact with infected bats or pigs, and by consuming contaminated food or drinks. Symptoms range from mild fever and headache to severe encephalitis, coma, acute respiratory syndrome, and death. As there is currently no specific treatment for NiV infection, prevention through proper hygiene methods and education are essential for curbing its spread.
The Current Progress of Nipah Virus Vaccine Development
The current progress of Nipah Virus (NiV) vaccine development has been encouraging. With ongoing research efforts, scientists have made substantial progress towards successfully developing an effective vaccine against this deadly virus. Several promising candidates have been designed using a variety of technologies including subunit vaccines, DNA vaccines, recombinant live-attenuated vaccines, and whole-inactivated vaccines. In addition to laboratory experiments conducted on animals such as mice and guinea pigs, many clinical trials are being conducted around the world to assess the safety and immunogenicity of these candidate vaccines against NiV infection in humans. These trials have demonstrated good results regarding immunity levels produced from the various vaccine formulations.
One notable example is a Phase I study conducted at Oxford University that showed that patients vaccinated with a DNA-based vaccine had significantly increased antibody responses compared to those who received placebo doses. This suggests that vaccination with this type of vaccine could provide protection against Nipah infections in people exposed to it. Other successful studies involving candidate vaccines have also been completed recently by organizations such as Merck Sharp & Dohme Corp., GlaxoSmithKline Biologicals SA., Takeda Pharmaceutical Company Limited., National Institute of Virology., etc. All these studies indicate that significant progress has been made towards the development of an effective Nipah Virus vaccine for use in humans.
But despite this progress it is important to note that much work still needs to be done before an approved NiV vaccine can become available for public use. Research efforts must continue so that scientists can understand how best to target this virus and develop an effective protective measure against it. In addition, governments around the world must invest resources into developing better diagnostics tools so as to identify cases early on before they can spread further. In conclusion, although considerable strides have been made towards creating an effective Nipah Virus Vaccine over the past few years, much more work still needs to be done before we can safely say that we now have a reliable means of preventing NiV infections in humans. It is thus essential for governments around the world to continue investing resources into researching this virus so that we may one day soon gain control over it and save countless lives from its devastating effects.
The Current Vaccine Development Process
The development of a Nipah Virus Vaccine has been a highly anticipated but intricate endeavor. Vaccines are among the most effective and economical approaches to prevent disease. As such, a lot of effort is put into designing safe and efficacious vaccines for Nipah virus that can be made available globally.
Before a vaccine can be designed, scientists must identify potential antigens – molecules which trigger an immune response – that can be used in the vaccine’s composition. These antigens may come from different parts of the virus or bacteria that cause the disease, such as its surface proteins or even pieces of its genetic material.
Preclinical testing
Once potential antigens have been identified, scientists move on to preclinical testing to assess how effective the vaccine will be at preventing infection in humans. In this stage, vaccines are tested on laboratory animals to determine their safety and efficacy. This helps researchers understand how well the vaccine works under various conditions before it is ready for human trials.
Clinical trials
The next step is clinical trials where humans are tested with the experimental vaccine in order to further assess it’s safety and efficacy. Clinical trials also provide important information about any side effects associated with taking the vaccine and whether it will protect against infection better than existing treatments or preventative measures. It typically takes several years for clinical trials to be completed before a vaccine is approved by regulatory agencies like Food and Drug Administration (FDA).
Production and distribution
Once approved by regulatory agencies, vaccines are then made available to the public through production and distribution channels such as pharmacies, clinics, health care providers, hospitals etc. This process usually takes several months or more depending on how quickly manufacturers can produce enough doses for global distribution.
The current progress of Nipah virus vaccine development is still in preclinical stages since there have not yet been any clinical trials for this particular virus due to lack of resources and funding. However, researchers are optimistic about making progress in developing one soon given its potential global impact on public health prevention efforts against Nipah virus outbreaks.
Challenges Faced by Researchers Working on NiV Vaccine Development
Developing a Nipah Virus (NiV) vaccine is an immense challenge for researchers. The virus spreads from animals to humans and even through direct contact with infected people, making it difficult to contain. In addition, NiV has a high mortality rate as there are no effective treatments or vaccines currently available. Furthermore, NiV has a short incubation period, which means it can rapidly spread from one person to another before the symptoms are visible. Additionally, scientists are still trying to understand the mechanism of how this virus works and the impact of its infection on humans. As such, there is no clarity about what type of vaccine would be most effective in fighting this virus.
In order to create an effective vaccine against Nipah Virus (NiV), researchers must first be able to identify the right kind of antigen which can successfully trigger an immune response in humans. Furthermore, creating a vaccine requires extensive testing and evaluation for safety and effectiveness before it can be approved for use by regulatory authorities like the USFDA or EMA. This makes the process long and expensive, leading to challenges in getting adequate funding for further research on developing a NiV vaccine. Moreover, since vaccines are given to healthy people, stringent safety protocols must be followed in order to ensure that any potential side effects will not cause harm.
Finally, as different countries have different standards of healthcare and access to medical resources, there may be discrepancies between results obtained from trials conducted in developed countries versus those conducted in developing countries where access is more limited. This could lead to additional difficulties when trying to obtain licensing approval for use globally. In conclusion, while scientists have made progress towards developing a NiV vaccine over the years, there are many challenges that they continue to face along their journey. They need adequate funding along with support from regulatory authorities as well as healthcare systems worldwide in order bring their efforts closer towards success.
Potential Solutions to These Challenges
Nipah Virus Vaccine development is a major area of focus in the global health sector with considerable research ongoing to develop a safe and efficient vaccine. To meet this challenge, various approaches are being explored to create a viable solution for this deadly virus. Currently, there are two primary potential solutions being considered – traditional vaccine development and the use of gene editing technology. Each has its own advantages and drawbacks that must be carefully weighed before a definitive path forward can be chosen.
The traditional approach to developing vaccines involves creating an attenuated live virus or using killed viruses as inert components to stimulate an immune response in the body. This is the same process that has been used for many years with great success. Unfortunately, it is not ideal for use against Nipah virus due to its rapid evolution and its ability to mutate quickly, making it difficult to predict which strain of the virus will be most effective at eliciting immunity. Nevertheless, research efforts are ongoing in this direction and there have been promising results thus far.
The other potential solution is gene editing technology, which allows scientists to modify existing viruses so they can elicit an immune response without causing illness or disease symptoms. This approach has been successfully used with other infectious agents such as Zika and Dengue fever in recent years, suggesting a promising future for Nipah vaccines as well. However, there are still numerous safety concerns associated with gene editing technologies that need to be addressed before they can be used widely in humans.
Both approaches have their own unique advantages and disadvantages that must be carefully weighed before any decisions can be made about which method should ultimately be pursued for Nipah Virus Vaccine development. The current progress of research towards developing an effective vaccine suggests that either of these potential solutions could lead to a successful outcome in the near future.
Impact of NiV Vaccine Development on Global Public Health
Nipah Virus Vaccine is a major area of focus for medical professionals and scientists around the world. It promises to be the solution to one of the most dangerous viral diseases that can affect humans – Nipah Virus. The virus, which has claimed over 300 lives in India and caused serious illness in Malaysian fruit bats, is highly contagious and can cause fatal neurological symptoms in humans. As such, it is essential that researchers continue to work towards developing a safe and effective vaccine against the virus. At present, there are several promising vaccines that have been developed to combat Nipah Virus. In Malaysia, researchers are working on a vaccine that is based on an attenuated strain of the virus, which has been shown to be safe and effective in animal trials. In India, scientists are studying a recombinant DNA-based vaccine which is capable of eliciting strong protective immunity against the virus. Additionally, researchers at Johns Hopkins University have recently created a new chimeric vaccine containing genes from both Nipah Virus and another virus called Hendra – this too has shown promise in animal studies.
Each of these vaccines presents its own unique benefits and drawbacks. The attenuated strain of Nipah Virus used in Malaysia may not induce long-term protective immunity, while the DNA-based vaccine in India may not offer complete protection from all forms of the virus. The chimeric vaccine developed by Johns Hopkins remains unproven but could offer greater protection than other vaccines if proven successful. The development of an effective vaccine against Nipah Virus has far-reaching implications for global public health as well as for public health policy makers – it would go a long way towards protecting people who live or travel through areas where cases of Nipah Virus have occurred, as well as those who work with infected animals or consume contaminated food products such as raw date palms or fruits bathed in saliva contaminated with the virus.
It also provides an opportunity for health care professionals to develop better ways to diagnose and treat this disease before it becomes deadly, thus reducing mortality rates associated with this infection worldwide. Finally, it gives hope to affected families that they may one day be able to protect their loved ones from harm due to this disease without having to resort to costly treatments or interventions that may not work. In conclusion, while much progress still needs to be made before an effective Nipah Virus Vaccine could become available for public use, current research continues to give us reason for optimism about its potential impact on global public health.