Researchers develop affordable, rapid blood test for brain cancer
A new, automated tool created by researchers at the University of Notre Dame can diagnose glioblastoma, a brain cancer that is rapidly spreading and incurable, in less than an hour. After diagnosis, glioblastoma patients typically live for 12 to 18 months.
The key component of the diagnosis is a biochip that detects biomarkers, or active Epidermal Growth Factor Receptors (EGFRs), which are located in extracellular vesicles and overexpressed in several malignancies, including glioblastoma. This biochip uses electrokinetic technology to detect biomarkers.
“Exosomes, also known as extracellular vesicles, are special nanoparticles that cells secrete. They have a weak charge and are large—between 10 and 50 times larger than a molecule. Hsueh-Chia Chang, the lead author of the study about the diagnostic published in Communications Biology and the Bayer Professor of Chemical and Biomolecular Engineering at Notre Dame, said, “Our technology was specifically designed for these nanoparticles, using their features to our advantage.”
The two tasks facing researchers were to identify a method for differentiating between active and inactive EGFRs and to design a diagnostic tool that could identify active EGFRs on extracellular vesicles from blood samples with a high degree of sensitivity and selectivity.
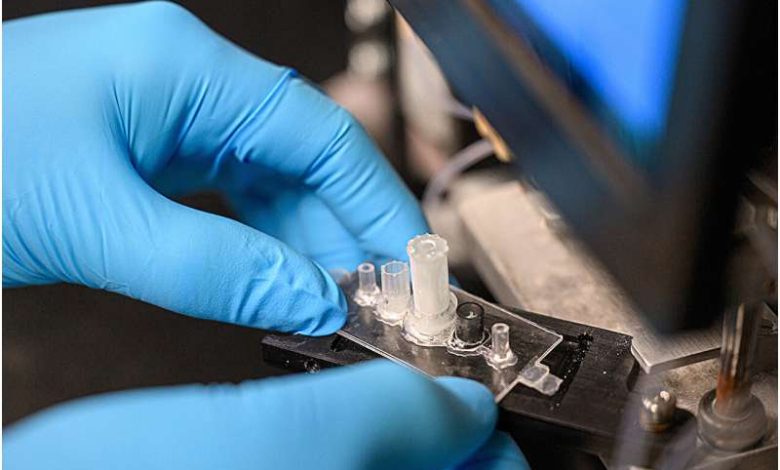
In order to achieve this, scientists developed a biochip that makes use of a cheap, electrokinetic sensor that is comparable in size to the ball in a ballpoint pen. Antibodies on the sensor can create many connections to a single extracellular vesicle because of their size. The diagnostic’s sensitivity and selectivity are greatly increased by this technique.
Subsequently, artificial silica nanoparticles with a strong negative charge “report” that the extracellular vesicles have active EGFRs. A voltage change is visible when extracellular vesicles containing active EGFRs are present, suggesting that the patient has glioblastoma.
This charge-sensing technique reduces interference, which is prevalent in sensor technologies that employ fluorescence or electrochemical reactions today.
According to co-author of the paper Satyajyoti Senapati, a research associate professor of chemical and biomolecular engineering at Notre Dame, “our electrokinetic sensor allows us to do things other diagnostics cannot.” Since our sensor is not impacted by other particles or chemicals, we may load blood straight away and extract the extracellular vesicles without the need for any pretreatment. Compared to other technologies, it exhibits minimal noise and increases our sensitivity for illness identification.”
The apparatus consists of three components in total: the biochip, a prototype of a portable machine that delivers test materials, and an automation interface. Although a new biochip is needed for each test, the prototype and automation interface can be reused.
It takes less than an hour to complete one test, and just 100 microliters of blood are needed. Less than $2 is needed in raw ingredients to produce one biochip.
The researchers claim that although though this diagnostic tool was created for glioblastoma, it can be modified to detect other kinds of biological nanoparticles. This makes it possible for the technology to identify various indicators for other illnesses. According to Chang, the group is investigating the use of technology in the diagnosis of pancreatic cancer as well as maybe other conditions like epilepsy, dementia, and cardiovascular disease.
“Our technique is not specific to glioblastoma, but it was particularly appropriate to start with it because of how deadly it is and the lack of early screening tests available,” said Chang. “Our hope is that if early detection is more feasible, then there is an increased chance of survival.”
The Centre for Research in Brain Cancer at the Olivia Newton-John Cancer Research Institute in Melbourne, Australia, contributed blood samples for the device’s testing.
Chang, Senapati, and former postdocs Sonu Kumar and Nalin Maniya from Notre Dame; Andrew Scott and Hui Gan from La Trobe University and the Olivia Newton-John Cancer Research Institute; and Jeffrey Franklin, James Higginbotham, and Robert Coffey from Vanderbilt University are among the other collaborators.




