A Disease That Makes Children Age Rapidly Gets Closer to a Cure
Progeria is an extremely rare condition for which there may soon be a treatment. Children affected by the condition have significantly shorter lifespans and age more quickly. However, there was no way to a really successful treatment until lately.
Now, using a cutting-edge gene editing method, a tiny group of government scientists and academics—among them Dr. Francis Collins, the former director of the National Institutes of Health—are working without expecting financial reward to stop progeria in its tracks.
Researchers claim that if gene editing proves successful in reducing or stopping progeria, it could also prove beneficial in treating other uncommon genetic diseases that lack cures or therapies and, similar to progeria, have not piqued the interest of pharmaceutical corporations.
Following 25 years of study, the team is contacting manufacturers and preparing to ask regulators for permission to conduct a progeria gene editing clinical trial.
According to Dr. Kiran Musunuru, a University of Pennsylvania gene editing expert who also provides advisory services to a gene editing startup, the idea “has merit, but also risk.” While the editing appeared to be effective in mice, he issued a warning that human patients may not have the same level of success.
In 1982, over thirty years before he was named director of the National Institute on Aging, Dr. Collins developed an interest in progeria while completing his study in medical genetics at Yale University. He saw Meg Casey, a new patient, one day. She was wrinkled like an older woman, hairless behind her wig, and less than four feet tall. It was only her twenties.
Progeria was her condition.
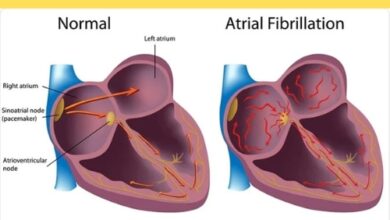
Dr. Collins felt touched and saddened. The condition, which affects only one in 18 to 20 million people, was almost unknown. Only 18 patients with progeria are known to be alive in the United States, according to the Progeria Research Foundation. People who have the disease frequently only live to be 14 or 15 years old, and many of them pass away from heart attacks or strokes. Ms. Casey and several other survivors have lived into their 20s.
Dr. Collins stated, “I thought, ‘Gosh, somebody should work on this.'” “I moved on to other things after that.”
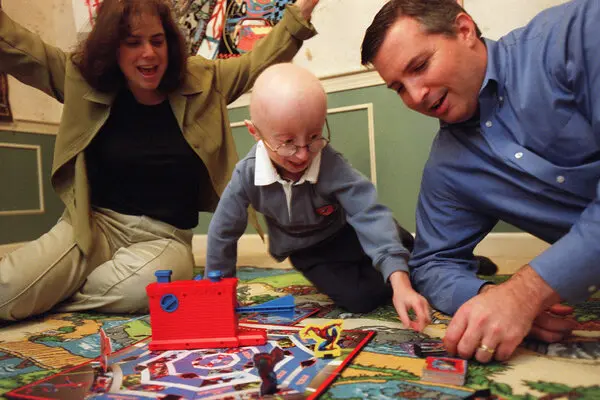
Nineteen years later, while attending a party, pediatric emergency department physician Dr. Scott Berns contacted Dr. Collins, who at the time was in charge of a federal effort to map the human genome. He disclosed to Dr. Collins the terrible illness that afflicted his toddler, Sam.
Dr. Berns remarked, “I don’t know if you’ve heard about it.” “We call it progeria.”
Dr. Collins said, “I do know a little bit about it.”
He recalled Casey, Ms.
Sam, age four, Dr. Collins, Dr. Berns, and his spouse, pediatric resident Dr. Leslie Gordon, were all welcomed to his home. Dr. Collins engaged Sam in a game of Frisbee while discussing the illness with his parents. Sam reached the age of seventeen.
Dr. Gordon informed Dr. Collins that although the condition was intriguing, its rarity made research on it a low priority. In order to fund promising research, she, Dr. Berns, and her sister Audrey—a lawyer—founded the Progeria Research Foundation.
She stated, “There was nothing else.”
Dr. Collins felt motivated. He was an administrator at the N.I.H., but he had his own modest lab where he could pursue any subject he chose to investigate. He made the choice to adopt progeria.
However, it took years for the possibility of a progeria treatment to become plausible, along with the advent of a new era in molecular medicine with advancements in gene editing.
According to Dr. Collins, the new forms of genome editing are “possibly the answer to a dream we all want to come true.” “The mutation for about seven thousand genetic diseases is known.”
85 percent of these hereditary illnesses are extremely rare, impacting less than one person out of every million.
And of them, “just a few hundred have treatments,” according to Dr. Collins.
“How about we give it a year?” he asked her.
That proved to be the simple part. Maria Eriksson, the man, needed only a few months to complete it. One letter out of the three billion distinct letters that make up human DNA—each one being a G, A, C, or T—was altered. One of those letters gets swapped out for another at a specific location in a gene called lamin A. As a result, the harmful protein progerin is produced, upsetting the scaffolding that maintains the normal shape of the cell nucleus.
An explanation of the discovery was presented in a 2003 publication by Drs. Eriksson, Collins, and colleagues.
Before conception, a sperm or egg cell has a mutation in lamin A. It’s just a random stroke of very bad luck.
After a few divisions, cells with the abnormal progerin begin to degrade and take on an increasingly strange appearance. The cells eventually receive a signal to self-destruct as a result of the degradation.
The lamin A mutation was then introduced into mice as the next stage of the study. The animals experienced rapid aging, heart illness, wrinkles on their skin, and hair loss, just like humans with the same disease. They also passed away young.
However, it wasn’t until 2012—when the DNA-cutting technique CRISPR—that the small study team believed a daring new medicine could be developed. Through DNA slicing, CRISPR can turn off a gene. That was far from ideal, though; a gene-repairing tool was actually what was required.
The Harvard professor David Liu, who directs the Merkin Institute for Transformative Technologies in Healthcare, came up with the answer in 2017. His team created a gene editing device that functions at the location of a mutation like a pencil. An enzyme is used to replace the DNA letter A with the letter G, guanine, at the site of the mutation. That is precisely what is required to fix the mutation in progeria.
There is never a trace of that gene editing enzyme in nature. Despite this, Nicole Gaudelli, a postdoctoral researcher in Dr. Liu’s group at the time, created one via a survival-of-the-fittest experiment in which she made bacteria manufacture the enzyme or perish. (Dr. Liu is a co-founder of other gene editing startups targeting more prevalent illnesses.)
Because the method his group developed directly modifies the bases—the letters that make up DNA—Dr. Liu dubbed it “base editing.”
Graduate student Luke Koblan, who works in Dr. Liu’s lab, attempted to correct the progeria mutation in patient cells cultured on petri dishes in one test. His test was successful.
Dr. Liu was ecstatic. Having viewed films on progeria, he was moved by the stories of the patients.
Dr. Liu received an invitation to speak at the N.I.H. in 2018. Since he was aware that Dr. Collins would be present, he included several slides about base modifying progeria patient cells.
Doc Collins was enthralled. To let her know what he had heard, he gave Dr. Gordon a call.
It resembled a lightning strike, according to Dr. Gordon.
Finally, there was genuine optimism.
“Oh my gosh, let’s go,” Dr. Collins recalls saying.
The Difficult Section
Initially, N.I.H. researchers aimed to enhance the well-being of progeria-ridden mice. They began by tentatively injecting just one basic editor.
As reported in a 2021 study, the outcomes considerably beyond their cautious expectations. Large heart artery damage, a defining feature of the illness, was nearly entirely repaired. The mice appeared to be in good health. Their hair was retained. And instead of passing away at 215 days from progeria, they survived to be roughly 510 days old, the beginning of old age in mice.
The gene editor was too big to be given to cells in a single molecular carrier, so Dr. Liu’s team had to reduce its size to expedite manufacture and reduce any possible negative effects of the delivery mechanism. That was a big order because there isn’t a single delivery method that can accommodate the original DNA-cutting CRISPR scissors system found in nature.
After achieving the shrinkage, the scientists had to test the novel gene editing enzyme in mice to determine whether the editing remained effective. Yes, it was.
Currently, a longer trial is being conducted to discover if the mice survive into old life.
The researchers are working out the next steps to apply their advances to treat progeria in youngsters as they wait. Every Monday at 4 p.m., the team convenes via Zoom.
Seeking approval from the Food and Drug Administration to initiate a clinical trial is their aim.
Locating a manufacturing partner to create the base editor for human use would be a crucial step.
Dr. Collins stated, “We hope to begin this trial in two years or less.”
And if it does succeed? If base editing for progeria paves the path for the thousands of other hereditary illnesses that currently lack a cure?
“Then, whoa,” remarked Dr. Collins.