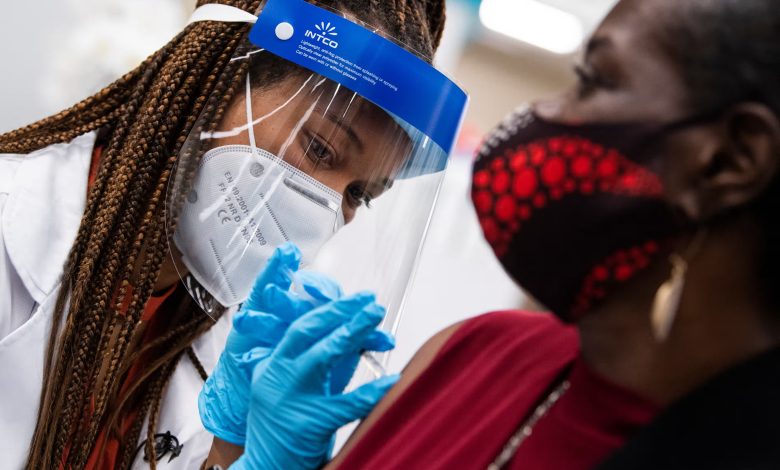
Covid surges in US as unequal access plagues vaccination and treatment rates
Data shows overall resistance to masks, but lower Paxlovid prescription and vaccination rates for people of color
Sewage statistics from the US Centers for Disease Control and Prevention (CDC) show that Covid is on the rise in the US, with levels of the virus expected to surpass the wave that occurred last summer nationally and go close to the height of the wave that occurred last winter in the west.
However, because to unequal availability, vaccination and antiviral adoption have remained low, and resistance to additional precautions like mask use is growing.
According to Dr. Peter Chin-Hong, an infectious disease specialist and professor of medicine at the University of California, San Francisco, “a lot of people are getting Covid right now all over the country.” “It’s tragic that there are still hospital admissions and a few hundred deaths in the US every week.”
Three variations that appear to be highly transmissible and immune-evading—dubbed Flirt due to common mutations—are driving the rise. Additionally, a large portion of the US has been experiencing heatwaves, and many people have stayed inside to avoid the heat, which could increase the virus’s spread.
Over the previous week, the number of Covid-related ER visits rose by 15.7% nationwide. This summer’s rising hospitalization rates are greater than they were this time last year, however it can be challenging to draw comparisons because a lot fewer hospitals are now obligated to disclose Covid rates than in prior years.
Moreover, mortality are rising after hitting the pandemic’s lowest point. The week ending June 12, the latest week for which complete statistics was available, saw over 400 deaths. In the US, COVID is still the fourth most common cause of death.
“With the tools at our disposal, any hospitalization or death could be totally avoided,” Chin-Hong declared.
Nonetheless, in contrast to previous surges, “it just feels like a very different time right now,” according to Harvard Medical School professor of healthcare policy David Grabowski. Even in hospitals and assisted living facilities, it is extremely uncommon to walk into a building and see people with masks.
According to experts, the summer spike coincides with a shift in federal and state policies away from measures that could halt the virus’s spread.
Recently, North Carolina passed legislation prohibiting the wearing of face masks in public, and representatives in New York City and Los Angeles have given the idea some thought as well.
The CDC relaxed its Covid isolation rules in May, advising patients to remain at home until their fever has subsided and their symptoms are improving, even if they are still positive for the virus and hence potentially contagious during that time.
The cost of the Covid vaccine was formerly paid by the US government, but starting in 2023, it was put on the private market. Weeks before the new booster becomes available, a bridging program that provided immunizations to uninsured individuals is coming to an end next month. This will probably make gaps in access to these potentially life-saving vaccines worse.
much though there is a danger of serious sickness, problems, and prolonged Covid because of Covid infection during pregnancy, only 22.5% of adults and 14.4% of children have received all recommended Covid vaccinations. The percentage among pregnant women is much lower, at 13.3%.
Additionally, there are notable differences among Americans of color, where disparities in access to healthcare still have an impact on vaccination rates. Only 15.6% of adults who identify as Indigenous and 16.2% of adults who identify as Hispanic had received the most recent booster shot, compared to 25% of adult whites.
Chin-Hong described the differences as “quite striking,” adding that older individuals of color, who have been more vulnerable to the pandemic, should be particularly concerned about them. “Making sure that all older populations receive vaccinations and understand their ability to keep people safe is not receiving as much attention.”
Although older persons have the highest risks of hospitalization and mortality, vaccination rates are greater among them; however, Grabowski stated that “those numbers are way too low.” Of those living in nursing homes, less than one-third had received their Covid shots in a timely manner.
“Those figures truly concern me.” He stated, “It’s unclear if those locals will be as safe as they were early in the pandemic.
Grabowski, who recently wrote on the measures required to make nursing homes safer following the epidemic, stated, “I think there’s a lot of fatigue around this issue, and I say that both among the staff and the residents.” “It seems like there isn’t the same level of caution as there was early in the pandemic.”
Similar uneven distribution has been seen with antivirals such as Paxlovid. Compared to white patients, people of color are much less likely to receive a Paxlovid prescription: 20% to 36% fewer in one study, and 30% to 36% fewer in another.
One pre-print study indicates that just 15% of patients at high risk of severe disease take Paxlovid, despite evidence that it helps prevent the worst outcomes, including death, among susceptible individuals.
Grabowski expressed his disappointment, saying, “It seems like we’re not really directing resources to the most vulnerable among us.” “That really raises red flags.”
Unlike viruses like the flu and RSV, which typically peak in the winter, Covid can increase at any time of the year, including summer, according to a recent explanation from the CDC.
According to the agency’s recommendation, booster shots should be updated for everyone over six months old in the fall and for everyone over 65, at least four months later.
When the new boosters become available in the fall, Chin-Hong anticipates that vaccination rates will climb once more. He also believes that public perceptions will change and that Covid immunizations will become as commonplace as flu injections. “Hopefully, a combo flu and Covid vaccine will be available in 2025,” he stated. “People might find it more palatable that way.”
Beyond vaccinations and treatments, efforts will also be necessary to prevent the virus’s transmission as it continues to circulate, especially in high-risk settings like nursing homes, according to Grabowski.
He declared, “We need to take additional steps, like testing, PPE, and improved air quality.” Still, Grabowski noted that progress has been sluggish and that many achievements made during the pandemic appear to be undone at this point.
“I believe that today, all of the planning that we had in place earlier in the pandemic is missing.”




