Multidrug Resistant TB Causes, Symptoms, Diagnosis and Treatment
What is Multidrug Resistant TB?
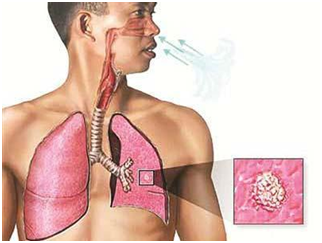
Tuberculosis (TB) is an infectious disease caused by a germ called Mycobacterium tuberculosis. Tuberculosis is spread through the air when a person sneezes, coughs, or breathes. Multi-Drug Resistant Tuberculosis (MDR-TB) is resistant to at least two of the main “first-line” drugs used to treat TB. TB may also be extensively drug-resistant (XDR-TB) which are strains that are resistant to two or more of the “second-line” drugs. Multidrug-resistant tuberculosis (MDR-TB) is tuberculosis due to organisms which show high-level resistance to both Isoniazid and Rifampicin, with or without resistance to other anti-TB drugs
Causes of Multidrug Resistant TB
There are two ways that people get Multidrug Resistant TB.
•Firstly, people get acquired drug resistant TB when their TB treatment is inadequate. This can be for a number of reasons, including the fact that patients fail to keep to proper TB treatment regimes. It can also be that the wrong TB drugs are prescribed, or sub standard TB drugs are used for treatment.
•Secondly, transmitted or primary drug resistant TB, results from the direct transmission of drug resistant TB from one person to another.
Symptoms of Multidrug Resistant TB
The general symptoms of Multidrug Resistant TB disease include
- Sickness or weakness,
- Weight loss
- Fever
- Night sweats.
The symptoms of TB disease of the lungs may also include
- Coughing
- Chest pain
- Coughing up blood.
Diagnosis of Multidrug Resistant TB
Globally there is very limited capacity to rapidly diagnose drug resistant TB. Although some new TB tests are becoming available such as the Genexpert TB test, point of care testing is still practically nonexistent in the areas with the highest TB burden. To overcome the problems of drug resistant TB there needs to be development of true point of care drug susceptibility tests, and their widespread implementation at affordable cost
Treatment of Multidrug Resistant TB
Multidrug-resistant (MDR) and extensively drug-resistant (XDR) tuberculosis are generally thought to have high mortality rates. However, many cases can be treated with the right combination and rational use of available ant tuberculosis drugs. The recommended regimen is the combination of at least four drugs to which the Mycobacterium tuberculosis isolate is likely to be susceptible. Drugs are chosen with a stepwise selection process through five groups on the basis of efficacy, safety, and cost.
- The first group (the oral first-line drugs) high-dose Isoniazid, pyrazinamide, and ethambutol are thought of as an adjunct for the treatment of MDR and XDR tuberculosis.
- The second group is the fluoroquinolones, of which the first choice is high-dose levofloxacin.
- The third group are the injectable drugs, which should be used in the following order: capreomycin, kanamycin, then amikacin.
- The fourth group is called the second-line drugs and should be used in the following order: thioamides, cycloserine, and then aminosalicylic acid.
- The fifth group includes drugs that are not very effective or for which there are sparse clinical data. Drugs in group five should be used in the following order: clofazimine, amoxicillin with clavulanate, linezolid, carbapenems, thioacetazone, and then clarithromycin.
By : Natural Health News




