The Risk Factors For Long COVID Have Finally Been Revealed

Many people who have SARS-CoV-2 experience an uncomfortable few weeks of fever, coughing, and exhaustion. But in about 1 in 5 cases, the pain lasts for several months at a time.
It’s unclear what exactly makes certain people more susceptible to an acute infection that lasts for a long time after COVID.
A group of US-based specialists examined the medical records of 4,708 adult US patients who contracted SARS-CoV-2 between April 2020 and February 2023. After three months, or when the COVID-19 threshold for extended COVID-19 was reached, about one in five still experienced problems.
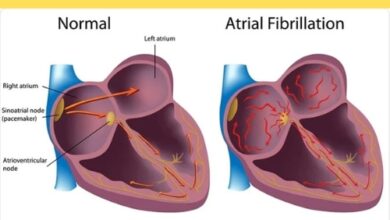
It was discovered that women and people with a history of cardiovascular disease were more likely to have long COVID. It was also less common in those with the less severe Omicron type of the virus and in those who had received vaccinations.
According to Elizabeth Oelsner, an epidemiologist at the Columbia University Irving Medical Center, “our study underscores the important role that vaccination against COVID has played, not just in reducing the severity of an infection but also in reducing the risk of long COVID.”
Longer recovery durations were associated with some medical disorders, such as a history of smoking and chronic obstructive lung disease, but these associations vanished when other risk variables were taken into account.
In addition to what is currently known about racial and ethnic differences with COVID-19, it was revealed that American Indian and Alaska Native individuals were more likely to have severe infections and require longer recovery durations.
Certain risk variables have been previously documented, such as a decreased risk for those who have had vaccinations and a higher long-term COVID risk for females. Even while prolonged COVID causes some profound alterations in the brain, the researchers in this group were unable to detect any evidence of a connection to mental health problems.
“Although studies have suggested that many patients with long COVID experience mental health challenges, we did not find that depressive symptoms prior to SARS-CoV-2 infection were a major risk factor for long COVID,” Oelsner says.
Researchers can more easily determine why long-term COVID is occurring in specific individuals and, consequently, what kinds of treatments may be useful in combating the illness, if they have a better understanding of who is most vulnerable to the disorder.
Even though the majority of the world is still trying to recover from the pandemic, millions of people worldwide who still have COVID-19 symptoms and society as a whole stand to gain from continued research into the illness.
“Our study clearly establishes that long COVID poses a substantial personal and societal burden,” Oelsner states.
“By identifying who was likely to have experienced a lengthy recovery, we have a better understanding of who should be involved in ongoing studies of how to lessen or prevent the long-term effects of SARS-CoV-2 infection.”
JAMA Network Open has released the research.